Cirrhosis
Cirrhosis is the endpoint in patients who have chronic progressive liver disease. Patients with abnormal liver function who develop ascites, variceal hemorrhage, hepatic encephalopathy,or renal impairment are considered to have end-stage liver disease (ESLD). While liver transplantation is a viable treatment option for ESLD, with increasing waiting times for organ transplantation, nearly 17% of patients on the transplant wait list die annually; others are not candidates for a liver transplant. Patients with ESLD have a constellation of symptoms and disease-related complications that affect survival and health-related quality of life.
What causes cirrhosis?
When a substance or disease attacks and damages the liver, liver cells are killed and scar tissue is formed. This scarring process is called fibrosis (pronounced "fi-bro-sis"), and it happens little by little over many years. When the whole liver is scarred, it shrinks and gets hard. This is called cirrhosis, and usually this damage cannot be undone.
Any illness that affects the liver over a long period of time may lead to fibrosis and, eventually cirrhosis. Some common causes are heavy drinking, viruses, a buildup of fat in the liver, inherited diseases, toxic effects from drugs and autoimmune diseases. These are more fully explored in the next section.
Cirrhosis has numerous causes. In the United States, heavy alcohol consumption and chronic hepatitis C have been the most common causes of cirrhosis. Obesity is becoming a common cause of cirrhosis, either as the sole cause or in combination with alcohol, hepatitis C, or both. Many people with cirrhosis have more than one cause of liver damage.
Cirrhosis is not caused by trauma to the liver or other acute, or short-term, causes of damage. Usually years of chronic injury are required to cause cirrhosis.
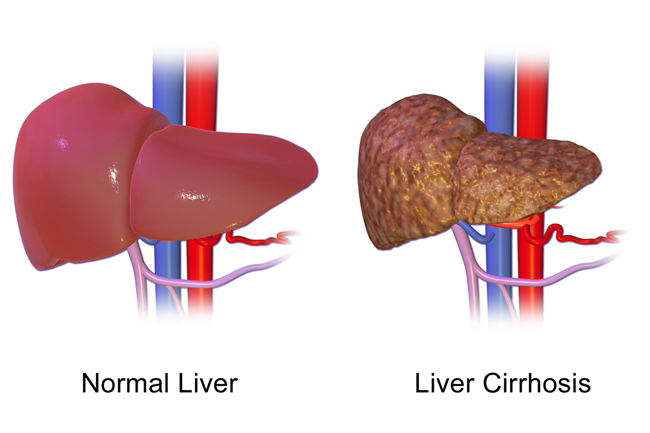
By BruceBlaus (Own work) [CC BY-SA 4.0], via Wikimedia Commons
Common Causes of Cirrhosis
| Alcohol-related liver disease. | Most people who consume alcohol do not suffer damage to the liver. But heavy alcohol use over several years can cause chronic injury to the liver. The amount of alcohol it takes to damage the liver varies greatly from person to person. For women, consuming two to three drinks-including beer and wine-per day and for men, three to four drinks per day, can lead to liver damage and cirrhosis. In the past, alcohol-related cirrhosis led to more deaths than cirrhosis due to any other cause. Deaths caused by obesity-related cirrhosis are increasing. |
| Chronic hepatitis C | The hepatitis C virus is a liver infection that is spread by contact with an infected person's blood. Chronic hepatitis C causes inflammation and damage to the liver over time that can lead to cirrhosis. |
| Chronic hepatitis B and D | The hepatitis B virus is a liver infection that is spread by contact with an infected person's blood, semen, or other body fluid. Hepatitis B, like hepatitis C, causes liver inflammation and injury that can lead to cirrhosis. The hepatitis B vaccine is given to all infants and many adults to prevent the virus. Hepatitis D is another virus that infects the liver and can lead to cirrhosis, but it occurs only in people who already have hepatitis B. |
| Nonalcoholic fatty liver disease (NAFLD) | In NAFLD, fat builds up in the liver and eventually causes cirrhosis. This increasingly common liver disease is associated with obesity, diabetes, protein malnutrition, coronary artery disease, and corticosteroid medications. |
| Autoimmune hepatitis | This form of hepatitis is caused by the body's immune system attacking liver cells and causing inflammation, damage, and eventually cirrhosis. Researchers believe genetic factors may make some people more prone to autoimmune diseases. About 70 percent of those with autoimmune hepatitis are female. |
| Diseases that damage or destroy bile ducts | Several diseases can damage or destroy the ducts that carry bile from the liver, causing bile to back up in the liver and leading to cirrhosis. In adults, the most common condition in this category is primary biliary cirrhosis, a disease in which the bile ducts become inflamed and damaged and, ultimately, disappear. Secondary biliary cirrhosis can happen if the ducts are mistakenly tied off or injured during gallbladder surgery. Primary sclerosing cholangitis is another condition that causes damage and scarring of bile ducts. In infants, damaged bile ducts are commonly caused by Alagille syndrome or biliary atresia, conditions in which the ducts are absent or injured. |
| Inherited diseases | Cystic fibrosis, alpha-1 antitrypsin deficiency, hemochromatosis, Wilson disease, galactosemia, and glycogen storage diseases are inherited diseases that interfere with how the liver produces, processes, and stores enzymes, proteins, metals, and other substances the body needs to function properly. Cirrhosis can result from these conditions. |
| Drugs, toxins, and infections | Other causes of cirrhosis include drug reactions, prolonged exposure to toxic chemicals, parasitic infections, and repeated bouts of heart failure with liver congestion. |
Complications of Cirrhosis
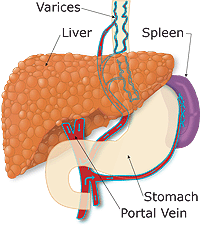
Because the liver becomes lumpy and stiff in cirrhosis, blood cannot flow through it easily, so pressure builds up in the vein that brings blood to the liver. This vein is called the portal vein. When pressure is high in the portal vein, the condition is called portal hypertension. In order to relieve this pressure, the blood passes through other veins. Some of these veins, called varices, can be found in the pipe that carries food from your mouth to your stomach (the esophagus) or in your stomach itself.
When a person has cirrhosis, the high pressure in the portal vein backs up into another organ called the spleen, which becomes enlarged and destroys an excessive number of platelets, the blood particles that help with blood clotting.

With cirrhosis, entrance of blood to the liver is blocked and substances such as ammonia that would normally be cleaned by the liver, escape into the general circulation.
Aside from the problems with liver blood flow, when cirrhosis is advanced there aren't enough healthy worker cells to get all the work done, so these cells cannot make the substances such as albumin and clotting factors that the liver normally makes.
Liver cancer, also known as hepatocellular carcinoma (HCC), can also develop in cirrhosis when some of the damaged liver cells start to multiply out of control. As liver function deteriorates, one or more complications may develop, often the first signs of the disease.
| Edema and ascites | When liver damage progresses to an advanced stage, fluid collects in the legs, called edema, and in the abdomen, called ascites. Ascites can lead to bacterial peritonitis, a serious infection. |
| Bruising and bleeding | When the liver slows or stops producing the proteins needed for blood clotting, a person will bruise or bleed easily. |
| Portal hypertension | Normally, blood from the intestines and spleen is carried to the liver through the portal vein. But cirrhosis slows the normal flow of blood, which increases the pressure in the portal vein. This condition is called portal hypertension. |
| Esophageal varices and gastropathy | When portal hypertension occurs, it may cause enlarged blood vessels in the esophagus, called varices, or in the stomach, called gastropathy, or both. Enlarged blood vessels are more likely to burst due to thin walls and increased pressure. If they burst, serious bleeding can occur in the esophagus or upper stomach, requiring immediate medical attention. |
| Splenomegaly | When portal hypertension occurs, the spleen frequently enlarges and holds white blood cells and platelets, reducing the numbers of these cells in the blood. A low platelet count may be the first evidence that a person has developed cirrhosis. |
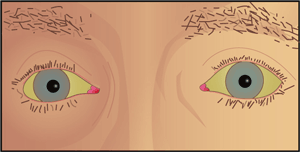
| Jaundice | Jaundice occurs when the diseased liver does not remove enough bilirubin from the blood, causing yellowing of the skin and whites of the eyes and darkening of the urine. Bilirubin is the pigment that gives bile its reddish-yellow color. |
| Gallstones | If cirrhosis prevents bile from flowing freely to and from the gallbladder, the bile hardens as gallstones. |
| Sensitivity to medications | Cirrhosis slows the liver's ability to filter medications from the blood. When this occurs, medications act longer than expected and build up in the body. This causes a person to be more sensitive to medications and their side effects. |
| Hepatic encephalopathy | A failing liver cannot remove toxins from the blood, and they eventually accumulate in the brain. The buildup of toxins in the brain-called hepatic encephalopathy-can decrease mental function and cause coma. Signs of decreased mental function include confusion, personality changes, memory loss, trouble concentrating, and a change in sleep habits. |
| Insulin resistance and type 2 diabetes | Cirrhosis causes resistance to insulin-a hormone produced by the pancreas that enables the body to use glucose as energy. With insulin resistance, the body's muscle, fat, and liver cells do not use insulin properly. The pancreas tries to keep up with the demand for insulin by producing more, but excess glucose builds up in the bloodstream causing type 2 diabetes. |
| Liver cancer | Hepatocellular carcinoma is a type of liver cancer that can occur in people with cirrhosis. Hepatocellular carcinoma has a high mortality rate, but several treatment options are available. |
| Other problems | Cirrhosis can cause immune system dysfunction, leading to the risk of infection. Cirrhosis can also cause kidney and lung failure, known as hepatorenal and hepatopulmonary syndromes. |
Symptoms of Cirrhosis
Initially, a person may have no symptoms at all. This is called compensated cirrhosis. In fact, a person may live many years with cirrhosis without being aware that his or her liver is scarred. This is because the pressure in the portal vein is not yet too high and there are still enough healthy liver cells to keep up with the body's needs.
However, if nothing is done about the cause of cirrhosis, (continuing to drink heavily, for example) or if the underlying disease such as hepatitis goes untreated, the pressure in the portal vein may increase to the point where the few remaining worker cells are overwhelmed. As cirrhosis progresses, the most common symptoms are:
- weakness
- fatigue
- loss of appetite
- nausea
- vomiting
- weight loss
- abdominal pain and bloating when fluid accumulates in the abdomen
- itching
- spiderlike blood vessels on the skin
Decompensated Cirrhosis
Cirrhosis is said to have progressed from compensated to decompensated cirrhosis when serious conditions develop as it worsens. These complications can be life-threatening and requires a new liver to replace the diseased one through a liver transplant. As discussed earlier, another serious complication of cirrhosis is liver cancer, which may occur in the compensated or decompensated stage. There may be no signs of liver cancer until the tumor i slarge and causing pain.
| Bleeding Varices | Internal bleeding from large blood vessels in the esophagus |
| Ascites | A buildup of fluid in the belly. (pronounced "a-sigh-tees") |
| Encephalopathy | Confusion from the buildup of toxins in the blood. (pronounced "en-sef-a-lop-a-thee") |
| Jaundice | Yellowing of the eyes and skin |
Bleeding varices (internal bleeding)
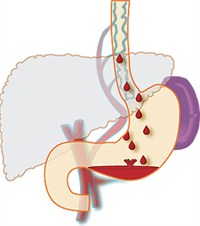
Large blood vessels (varices) in the food tube get bigger and bigger over time and can burst open. When this happens, a person may vomit blood or have stool that is black and tarry.
The risk of bleeding from varices can be reduced by blood pressure medicines known as beta-blockers or by a surgical procedure in which tiny rubber bands are tied around the varices.
Ascites (fluid in the belly)

Another problem caused by high pressure in the veins of the liver is ascites. Fluid leaks out into the belly and it begins to fill it up. This can make the abdomen enlarge like a balloon filled with water. The legs can get swollen too. This can be very uncomfortable.
Eating can be a problem because there is less room for food. Even breathing can be a problem, especially when the person is lying down. But the most dangerous problem with ascites is infection, which can be life-threatening.
Ascites may go away with a low salt diet, and with diuretics (water pills) ordered by your provider. But sometimes a provider must actually drain the fluid from the belly using a special kind of needle.
Encephalopathy (confusion)
A liver that is working poorly may not be able to get rid of toxic substances like ammonia (which comes from the intestines), and it may allow these substances to go into the brain and cause confusion.

Besides confusion, toxins in the brain cause changes in sleep, mood, concentration, and memory. If extremely serious, it can even cause a coma. These are all symptoms of hepatic encephalopathy. With encephalopathy, a persons may have problems driving, writing, calculating, and performing other activities of daily living.
Signs of encephalopathy are trembling and hand "flapping." Encephalopathy may occur with an infection or internal bleeding, if constipated or with overuse of water pills or take tranquilizers or sleeping pills.
Jaundice (yellowing of eyes and skin)
A liver that is working poorly cannot get rid of bilirubin, a substance that produces a yellowing of the eyes and skin called jaundice. Too much alcohol and some medicines can also lead to jaundice.
How is the severity of cirrhosis measured?
The model for end-stage liver disease (MELD) score measures the severity of cirrhosis. The MELD score was developed to predict the 90-day survival of people with advanced cirrhosis. The MELD score is based on three blood tests:
- international normalized ratio (INR)-tests the clotting tendency of blood
- bilirubin-tests the amount of bile pigment in the blood
- creatinine-tests kidney function
MELD scores usually range between 6 and 40, with a score of 6 indicating the best likelihood of 90-day survival.
How is cirrhosis diagnosed?
The diagnosis of cirrhosis is usually based on the presence of a risk factor for cirrhosis, such as alcohol use or obesity, and is confirmed by physical examination, blood tests, and imaging. The doctor will ask about the person's medical history and symptoms and perform a thorough physical examination to observe for clinical signs of the disease. For example, on abdominal examination, the liver may feel hard or enlarged with signs of ascites. The doctor will order blood tests that may be helpful in evaluating the liver and increasing the suspicion of cirrhosis.
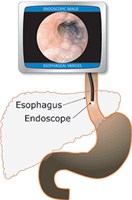
Patient with cirrhosis may have an upper endoscopy (pronounced "en-dahs-cup-ee") periodically (see figure at right). A thin tube with a camera can be inserted into the mouth to look for varices in the esophagus (food tube) and the stomach. The endoscopy is repeated every few years to monitor for varices.
To view the liver for signs of enlargement, reduced blood flow, or ascites, the doctor may order a computerized tomography (CT) scan, ultrasound, magnetic resonance imaging (MRI), or liver scan. The doctor may look at the liver directly by inserting a laparoscope into the abdomen. A laparoscope is an instrument with a camera that relays pictures to a computer screen.
A liver biopsy can confirm the diagnosis of cirrhosis but is not always necessary. A biopsy is usually done if the result might have an impact on treatment. The biopsy is performed with a needle inserted between the ribs or into a vein in the neck. Precautions are taken to minimize discomfort. A tiny sample of liver tissue is examined with a microscope for scarring or other signs of cirrhosis. Sometimes a cause of liver damage other than cirrhosis is found during biopsy.
How is cirrhosis treated?
Treatment for cirrhosis depends on the cause of the disease and whether complications are present. The goals of treatment are to slow the progression of scar tissue in the liver and prevent or treat the complications of the disease. Hospitalization may be necessary for cirrhosis with complications.
Eating a nutritious diet
Because malnutrition is common in people with cirrhosis, a healthy diet is important in all stages of the disease. Health care providers recommend a meal plan that is well balanced. If ascites develops, a sodium-restricted diet is recommended. A person with cirrhosis should not eat raw shellfish, which can contain a bacterium that causes serious infection. To improve nutrition, the doctor may add a liquid supplement taken by mouth or through a nasogastric tube-a tiny tube inserted through the nose and throat that reaches into the stomach.
Avoiding alcohol and other substances
People with cirrhosis are encouraged not to consume any alcohol or illicit substances, as both will cause more liver damage. Because many vitamins and medications-prescription and over-the-counter-can affect liver function, a doctor should be consulted before taking them.
Treatment for cirrhosis also addresses specific complications
For edema and ascites, the doctor will recommend diuretics-medications that remove fluid from the body. Large amounts of ascitic fluid may be removed from the abdomen and checked for bacterial peritonitis. Oral antibiotics may be prescribed to prevent infection. Severe infection with ascites will require intravenous (IV) antibiotics.
Portal Hypertension
The doctor may prescribe a beta-blocker or nitrate for portal hypertension. Beta-blockers can lower the pressure in the varices and reduce the risk of bleeding. Gastrointestinal bleeding requires an immediate upper endoscopy to look for esophageal varices. The doctor may perform a band-ligation using a special device to compress the varices and stop the bleeding. People who have had varices in the past may need to take medicine to prevent future episodes.
Hepatic encephalopathy
Hepatic encephalopathy is treated by cleansing the bowel with lactulose-a laxative given orally or in enemas. Antibiotics are added to the treatment if necessary. Patients may be asked to reduce dietary protein intake. Hepatic encephalopathy may improve as other complications of cirrhosis are controlled.
Some people with cirrhosis who develop hepatorenal failure must undergo regular hemodialysis treatment, which uses a machine to clean wastes from the blood. Medications are also given to improve blood flow through the kidneys.
Other treatments
Other treatments address the specific causes of cirrhosis. Treatment for cirrhosis caused by hepatitis depends on the specific type of hepatitis. For example, interferon and other antiviral drugs are prescribed for viral hepatitis, and autoimmune hepatitis requires corticosteroids and other drugs that suppress the immune system.
Medications are given to treat various symptoms of cirrhosis, such as itching and abdominal pain.
When is a liver transplant indicated for cirrhosis?
A liver transplant is considered necessary when complications cannot be controlled by treatment. Liver transplantation is a major operation in which the diseased liver is removed and replaced with a healthy one from an organ donor. A team of health professionals determines the risks and benefits of the procedure for each patient. Survival rates have improved over the past several years because of drugs that suppress the immune system and keep it from attacking and damaging the new liver.
The number of people who need a liver transplant far exceeds the number of available organs. A person needing a transplant must go through a complicated evaluation process before being added to a long transplant waiting list. Generally, organs are given to people with the best chance of living the longest after a transplant. Survival after a transplant requires intensive follow-up and cooperation on the part of the patient and caregiver.
Summary
- Cirrhosis is a condition in which the liver slowly deteriorates and malfunctions due to chronic injury. Scar tissue replaces normal, healthy liver tissue, preventing the liver from working as it should.
- In the United States, heavy alcohol consumption and chronic hepatitis C have been the most common causes of cirrhosis. Obesity is becoming a common cause of cirrhosis, either as the sole cause or in combination with alcohol, hepatitis C, or both. Many people with cirrhosis have more than one cause of liver damage.
- Other causes of cirrhosis include hepatitis B, hepatitis D, and autoimmune hepatitis; diseases that damage or destroy bile ducts, inherited diseases, and nonalcoholic fatty liver disease; and drugs, toxins, and infections.
- Many people with cirrhosis have no symptoms in the early stages of the disease. As the disease progresses, symptoms may include weakness, fatigue, loss of appetite, nausea, vomiting, weight loss, abdominal pain and bloating, itching, and spiderlike blood vessels on the skin.
- As liver function deteriorates, one or more complications may develop. In some people, complications may be the first signs of the disease.
- The goals of treatment are to stop the progression of scar tissue in the liver and prevent or treat complications.
- Treatment for cirrhosis includes avoidance of alcohol and other drugs, nutrition therapy, and other therapies that treat specific complications or causes of the disease.
- Hospitalization may be necessary for cirrhosis with complications.
- A liver transplant is considered when complications of cirrhosis cannot be controlled by treatment.